CRITICAL CARE PEARLS
by Allison Harriott, MD, MPH
Critical Care & Emergency Medicine Specialist
About
Allison Harriott, MD
Critical Care & Emergency Medicine Specialist
Dr. Allison Harriott is a distinguished double-boarded physician with an extensive background spanning over a decade in the fields of Emergency Medicine and Critical Care Medicine. Dr. Harriott completed residency training in Emergency Medicine at SUNY Downstate/Kings County Hospital Center in Brooklyn, NY, graduating in 2013. During this time, she exhibited exceptional dedication and a profound commitment to advancing medical education.

Dr. Allison Harriott's journey in medical education radiates with a luminescent dedication, her invitation to the esteemed ACEP Teaching Fellowship illuminating her path to a profound commitment to advancing patient well-being through her unparalleled teaching prowess.
Guiding the course of medical evolution, Dr. Harriott's presence in the realm of healthcare resonates as a symphony of expertise, as she imparts her artistry in procedural finesse and interdisciplinary harmony, crafting a legacy of compassion-driven healers ready to inscribe their mark on the tapestry of patient care.
Seminar
Advancing Patient Care Through Simulation-Based Training: A Comprehensive Seminar for Medical Professionals
DAY 1
Enhancing Team Dynamics in Emergency Care (8 hours)
Morning Session:
- 1. Introduction to Simulation-Based Learning (1 hour)
- 2. Building Effective Interdisciplinary Teams (1.5 hours)
- 3. Simulation Scenarios: Team-Based Approach (2 hours)
Afternoon Session:
- 4. Debriefing and Reflective Learning (1.5 hours)
- 5. Managing Challenging Situations as a Team (1.5 hours)
DAY 2
Mastering Critical Procedures with Simulation-Based Training (8 hours)
Morning Session:
- 1. Advanced Airway Management (2 hours)
- 2. Central Line Placement and Invasive Monitoring (1.5 hours)
- 3. Code Team Coordination and Crisis Resource Management (2 hours)
Afternoon Session:
- 4. Ventilator Management and Respiratory Emergencies (2 hours)
- 5. Hands-on Procedural Stations (1.5 hours)
Master Running Code Blues!

Most Important Factors
- Team Leadership
- Hemodynamic Directed Resuscitation
- High Quality CPR
- Early Defibrillation
- Medications
- Novel Therapies
- Post Arrest Care
Perfusion Protection Strategies in Mechanically Ventilated Patients
Physiology
- Normal intra-thoracic pressureis zero to negative
- Positive pressure ventilation (PPV) reverses this physiology, making intra-thoracic pressure positive
- Afterload Reduction
- Negative intra-thoracic pressure contributes to afterload
- PPV decreases afterload by increasing intra-thoracic pressure
- Negative intra-thoracic pressure contributes to afterload
- Hypovolemia
- Induction agents cause venodilation and decrease mean systemic pressure
Post-intubation hypotension
- Positive pressure ventilation + drugs → hypotension
- Incidence: 9.6-60%
- Predictors:
- Use of Neuro-muscular blockade – OR 2.7 (1.12-6.53)
- Pre-existing low mean arterial pressure – OR 1.25 (1.01-1.55)
- Shock index (HR/SBP) >0.8 – 67% sensitivity, 80% specificity
- ESRD
- Age
- mSI (HR/MAP) >1.3– more sensitive and specific than SI
Prevention
- Premedication: Fentanyl:Ketamine:Rocuronium (3:2:1 vs 1:1:1)
- Ketamine associated with less myocardial depression, less AV dissociation and arrhythmias
- Pre-intubation volume resuscitation
- Awake intubation
- Have a push-dose pure vasoconstrictor ready (phenylephrine, epinephrine)
- Proper PPV settings
- PEEP: 5
- Tidal Volume: 6-8 ml / kg PBW
Mastering Vasopressor Management
Rules of Critical Care
1. Defend the blood pressure
- “True” hypotension is an emergency
- MAP<65 needs attention IMMEDIATELY
- Hypotension →Decreased DBP → Decreased coronary blood flow → Cardiac ischemia → Decreased CO → Hypotension (repeat)
- Short durations hurt brain, kidneys, heart
- Longer durations of hypotension = worse outcomes
- Push dose, immediate fluids, etc.
- FIX IT!
- MAP<65 needs attention IMMEDIATELY
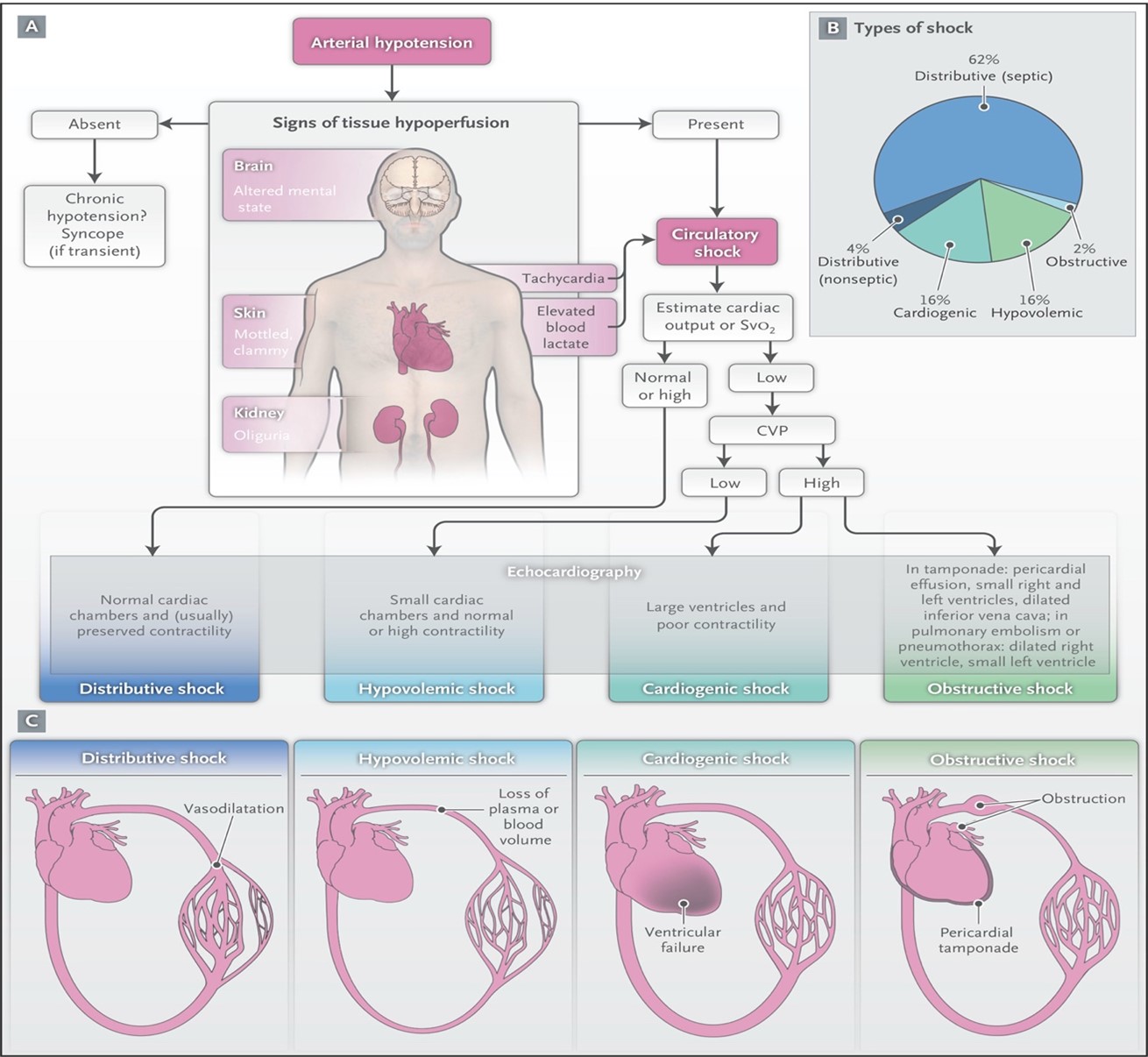
2. You MUST diagnose shock
- Always identify which type of shock!
- Stabilize/Defend BP
- Assessment of CO → Diagnose shock type
- Volume trial → Look for CO improvement
Mastering Mechanical Ventilation Basics
- Respiratory failure
- Goals
- Ventilator Definitions
- Waveforms
- Ventilator adjustments
- Troubleshooting
Sponsored by
The Critical Care Physicians and The Center for Peer Review Justice